Pizza tracker versus patient tracker
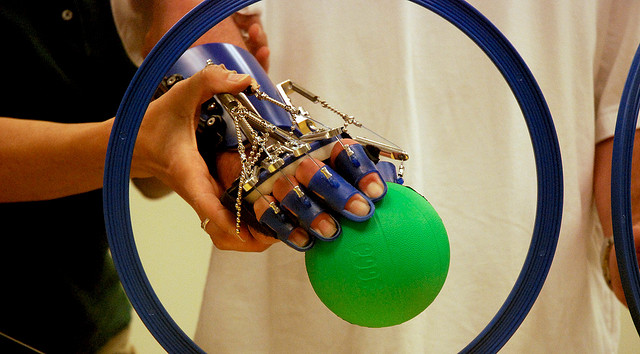
M. Bridget Duffy, M.D., is chief medical officer of Vocera Communications and co-founder of ExperiaHealth, a collaborative that seeks to humanize health care. Her post is part of our Knight News Challenge: Health series. The challenge, which offers $2.2 million in funding for ideas to help harness data and information for the health of communities, closes Tuesday, Sept. 17, at 5 p.m. ET. Photo credit: Flickr user KOMUNews.
Capturing data is great. But if doctors and patients cannot readily access and use data to optimize outcomes, what’s the point? The technology investment in how we capture and use “Big Data” says a lot about our priorities. RELATED LINKs
“What’s next in Knight News Challenge: Health” by Chris Sopher
“Bring your best ideas; deadline nears for News Challenge: Health” by Chris Sopher
“Knight News Challenge: Health opens with inspiration phase, additional prizes from collaborators” by Raina Kumra and John Bracken
“Announcing key collaborators and details of Knight News Challenge: Health” by John Bracken and Chris Barr
“Join us to brainstorm ideas around News Challenge: Health” and There’s still time to brainstorm around News Challenge: Heath” by Chris Sopher
“Data: Why we care” by Esther Dyson
“News Challenge: Make APIs not apps, health CEO says” by Lucky Gunasekara
“Data provides a focus for community action” by Bryan Sivak
“California HealthCare Foundation: The data stops here” and “It takes a community to humanize health data” by Andy Krackov
“How data-driven solutions can transform healthcare” by Lexie Komisar
“Data essential to promoting healthy habits” by Nirav R. Shah
If we have the technology to order a pizza and track its progress online, we should also invest in technology that can track a patient’s progress, tests and plan of care. Patients and health care providers must have access to the data they need to make informed decisions and improve medical outcomes, and that data must be communicated to patients in a way that eases the burden of illness versus adding to it. Why are we willing to spend $32 billion annually on the global pizza industry but hesitant to invest in technology to improve health care? That’s the question I pose when talking to other physicians, who, like me, want to leverage technology to humanize health care.
My journey to the intersection of health care and technology started more than 20 years ago during an aha moment in the last month of my residency training. I sat down at a patient’s bed and watched as every specialist came into the room and dealt with the machines and the data, but never interacted with the patient or his family. It was then that I realized the system was diseased and fragmented, and that technology was actually “dehumanizing” care. This was closely followed by a chance phone call that served as the catalyst to having me challenge the status quo in health care for the rest of my career.
I read a paper about Dr. Earl Bakken, founder of Medtronic and inventor of the pacemaker, who wrote about creating “the most healing hospital in America” 50 years ago. I called Earl and told him I wanted to help him build this hospital. He laughed and said he had retired to a hammock on the Big Island of Hawaii. Our conversation took an interesting turn as Earl described how, even though we were able to make great advances in medical technology (such as his pacemaker), he believed that only 20 percent of healing is actually linked to technology. The other 80 percent was linked to human-to-human interaction and communication, physical environment and spirituality. He challenged me to find ways to improve “the other 80 percent.” After that conversation he became my mentor and later my colleague as I joined Medtronic to tackle that challenge. Earl’s retirement was short-lived; the hospital he envisioned was built, and today serves as a model for the rest of the country.
My career became focused on restoring humanity to health care. I became the nation’s first chief experience officer (CXO) at the Cleveland Clinic and later co-founded ExperiaHealth, a health care technology and advisory firm that works with hospitals on improving patient and staff experience. As I discussed challenges one on one with care providers and patients and reviewed various solutions during our CXO roundtable forums with other like-minded physicians, I had another “Aha!” When we mapped the gaps in the human experience of care, we found that the No. 1 thing that was broken was communication. I realized that in order to fix the “80 percent” I really needed the “20 percent” technology component to improve communication and produce scalable long-term solutions. As my team and I began researching technology solutions, we began working with Vocera Communications. Vocera and ExperiaHealth had independently made the same discovery: The primary problem in patient and staff dissatisfaction, adverse outcomes and bureaucratic processes could always be traced back to communication. With Vocera’s technologies addressing the communication problem in health care and other mission-critical environments, and ExperiaHealth’s expertise in clinical workflows, health care laws and operational efficiencies, we knew we could utilize technology to get physicians and nurses back to their core mission: helping patients. I joined the board of Vocera and later became chief medical officer of the company.
In this role I have the opportunity to encourage other physicians to step up and lead. We help organizations to accelerate the adoption of integrated, intelligent communications that empower patients and care providers to create a path to optimal well-being. We also inspire and deploy health care innovations that I hope one day soon will include a patient data tracker. The returns are compelling: improved patient and staff satisfaction scores, better medical outcomes and a healthier balance sheet. For me and my fellow physicians, the technology enables us to have more meaningful interactions with our patients and restore joy to practicing medicine.
Knight Foundation has committed $2 million to News Challenge: Health. The Robert Wood Johnson Foundation will award prizes of $50,000, $30,000 and $20,000 respectively for the top three projects that “best combine public health data and health care data.” The California Health care Foundation will award $100,000 to one or more ideas that enhance the use of health data in local policymaking. For more visit newschallenge.org.
Recent Content
-
Journalismarticle ·
-
Journalismarticle ·
-
Journalismarticle ·


