One year later, award-winning series saves newborn lives
Ellen Gabler is an investigative reporter and assistant editor at the Milwaukee Journal Sentinel, and Allan James Vestal is a news applications developer at the Journal Sentinel. In 2014, Gabler and Vestal won a Livingston Award for their series “Deadly Delays,” an investigation on life-threatening delays in newborn blood testing. The series spurred dozens of states to make significant changes to address delays from keeping labs open on weekends to identifying problem hospitals and providing them with regular performance reports. The Livingston Awards are supported by Knight Foundation. Below, Gabler writes about their series. This story is cross-posted from The Huffington Post.
It took $7 and a tweak in hospital procedure to save Juniper Horrocks’ life. Had the baby been born just four days earlier, she likely would not have survived.
Juniper was born in October 2014 at a hospital in rural Utah. Just three days earlier, the hospital had started using FedEx to ship newborn screening samples overnight to Utah’s state lab. Previously, they used regular mail, which meant some babies blood samples took more than five days to get to the lab.
A wait like that could have killed Juniper. The baby has a genetic disorder that can be deadly if left untreated in the first few days of life.
Luckily for Juniper and her family, Utah had been revamping its newborn screening program in response to our Milwaukee Journal Sentinel investigation based on an analysis of nearly 3 million newborn screening tests from babies in 31 states.
The investigation found that thousands of babies’ blood samples from hospitals across the nation were arriving late at state labs, where they are to be quickly tested for genetic disorders that can be treated if caught early. Infants have died and suffered brain damage and other permanent disabilities because of screening delays by hospitals and state labs.
As a reporter with the Milwaukee Journal Sentinel, I use data to do investigations. My colleague, Allan James Vestal, builds news applications so people can easily explore the information.
Newborn screening is required throughout the country. Nearly every baby has their heel pricked within a day or two of birth. Spots of blood are collected on a filter card and that card is supposed to be sent within 24 hours to a state lab where it is tested for rare, yet deadly, disorders.
Hospitals sometimes batch the cards because it saves money. In other instances, hospitals haven’t established newborn screening protocols or staffers don’t follow them when they’ve been set.
These details matter for babies like Juniper, who has a genetic disorder called MCAD deficiency. A newborn with MCAD deficiency cannot properly convert some fats to energy. They can appear healthy while fatty acids are building up in the body, soon plunging the child into metabolic crisis. A baby who takes a nap and goes too long without eating can suddenly die or end up brain damaged. If the disorder is detected early, however, parents know to feed the child every two hours. That’s often all it takes for a baby to grow up and lead a normal, healthy life.
A science reporter had gotten a tip about a Wisconsin baby who had gotten sick and nearly died because his newborn screening sample was sent late. Was this a problem beyond one baby?
Those newborn screening cards that come into state labs must be tracked—that means data. I requested newborn screening data from Wisconsin first. Officials refused, saying it would be adversarial to hospitals to release the information. I decided to request the data from all 50 states while I battled with Wisconsin officials.
I spent five months negotiating for data from across the country. In most cases, state officials were reluctant to turn it over. Eventually, it was time to write the story. I had gotten data from 31 states and analyzed 3 million newborn screening tests.
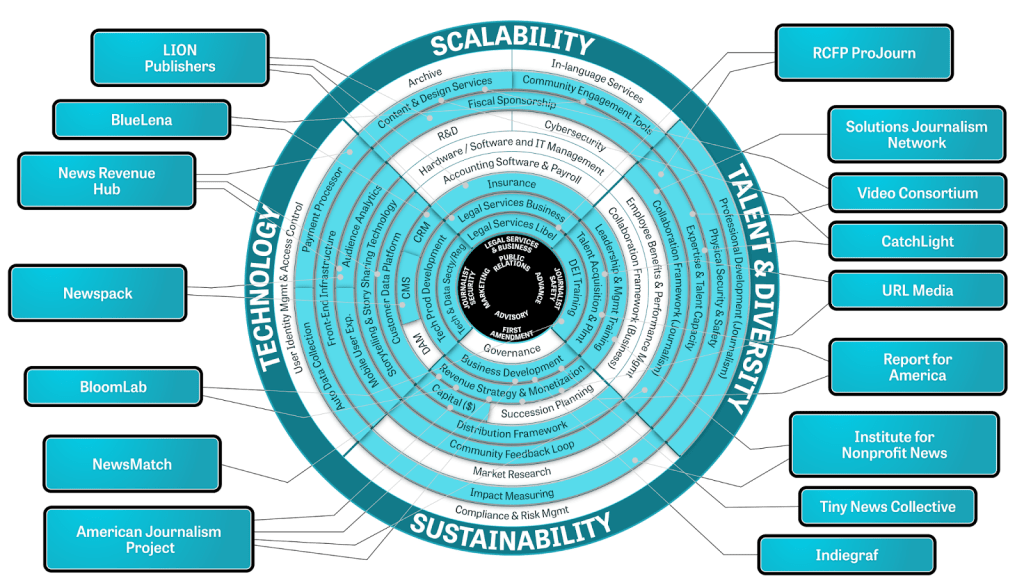
Using that data, Allan built this interactive graphic so parents could look up the performance of specific hospitals, see if their state’s lab is closed on the weekends (which adds to delays), and contact state officials to urge them to release data if they had not.
Results were immediate. Before the first story even published, the largest hospital chain in Wisconsin said it was changing its newborn screening protocol. Dozens of states and thousands of hospitals throughout the country have since dramatically changed how they approach newborn screening.
Arizona turned one of the country’s worst-performing newborn screening programs into one of the best. In 2013, just 67 percent of newborn screening samples were getting to the state lab within the federally recommended three days. About six months later, that was up to 99 percent.
Congress passed legislation that includes new timeliness and tracking measures for newborn screening to eliminate delays. These changes have been heartening. Hearing about Juniper was incredible.
Andy Rohrwasser, Utah’s newborn screening director, arranged for the poorest-performing hospitals to use FedEx to get samples to the state lab overnight. He shifted around other costs to pay the $7 it would cost per sample.
“Nobody really needed to tell me, ‘You must,’” Rohrwasser said. “It’s so obvious when you look at the data and the outcome. It’s not rocket science to see that we are not doing so hot. We can do much, much better.”
And they did.
“We are so incredibly lucky,” said Juniper’s mom, Jerrah Horrocks.’

Recent Content
-
Journalismarticle ·
-
Journalismarticle ·
-
Journalismarticle ·